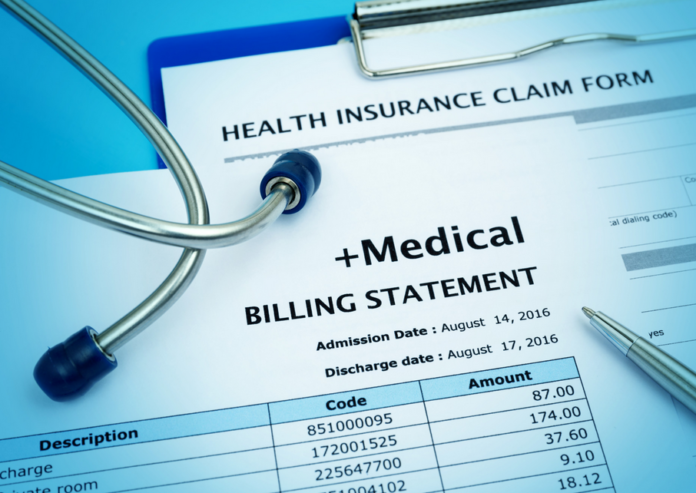
According to research, there are 92,703 medical coders employed in America.
The world of medical coding jobs can be confusing, and it’s hard to know where to start.
There are a lot of different things you need to know in order to be successful in medical coding. It can be overwhelming and confusing to try to learn everything on your own.
But don’t worry. Keep reading because our guide will introduce you to some of the key concepts in medical coding, and help you get started on your journey to becoming a successful coder.
1. Organization
Organization is one of the most important factors in any job because it makes everything faster and more efficient. In regards to medical coding you need to have everything organized for three reasons:
- So you don’t become overwhelmed by all the patient information
- So filing claims takes as little time as possible
- For easy retrieval, if specific records are questioned
Paper folders work well for medical billing, but if you have a large number of files going back several years it can be easy to misplace them.
A filing cabinet or the cloud is better for long-term storage and retrieval.
2. Accuracy and Speed
Any mistake will be reflected in the money you receive from the insurance company. That’s why maintaining accuracy is so important.
If you are off by one number or letter then that could equate to thousands of dollars lost every month.
Furthermore, it’s not just about getting the code right but also making sure that it is done within a certain timeframe.
This is important because most providers have limited time to file claims before an insurance company stops covering procedures for that patient.
It may also vary depending on what type of insurance plan they have so been specific is key when completing this task.
Also, the faster you can code patient records the more time you have to do other tasks. Medical coding doesn’t require a lot of manual data entry, so specialists should be able to handle 10 patients per hour.
Higher-end software can automatically fill out information from records into standard codes that are submitted with claims which cut down on the time required for coding.
The more accurate your coding is at first will save time when it comes time for billing since there’s less tweaking needed when submitting claims.
3. Familiarity with Procedures And Common E/M Coding
Having knowledge of procedures like patient visits (E/M coding) is critical in medical coding. The first thing you’ll need to do is find out what type of credentials your practice needs for reimbursement.
All insurance companies have different requirements so it’s important to know who will be paying for each visit so you can code accordingly.
For example, if an office sees patients on a sliding fee schedule then there are limited circumstances that allow them to bill insurance companies due to low-income status.
If that’s the case then the focus should be on collecting as much data as possible from each patient visit since most of it would not be reimbursed.
Another example is orthopedic medicine.
It’s important to document a patient’s progress related to any injuries or conditions with as much specificity as possible because reimbursement will be based upon the level of improvement.
For instance, if a doctor performs a procedure and eventually the next visit shows that the patient is doing better with less pain then you need to code it as “no change”.
4) Willingness to Ask for Help
To err is human and coding medical records accurately means there are going to be mistaken sometimes. Anyone who codes regularly knows that they cannot possibly memorize every single procedure that exists.
That means asking other people who may know more about specific procedures or getting help from someone at the insurance company can get you back on track faster.
While it may seem embarrassing to ask for help when medical coding, it’s important to remember that insurance companies are more understanding than you think when mistakes are made.
5) Ability to Stay Organized
As previously mentioned, organization is key in successfully completing any task related to medical billing and coding certification. When bills or medical records pile up it can be difficult to keep track of everything.
This is why having a filing system in place is necessary. This will also allow you to prioritize tasks like billing your orthopedic practice.
6) Flexible Schedule
Being able to work flexible hours may not seem like an important factor. But someone who works 9-5 every day will not be able to get the most out of medical coding.
This is due to the fact that each insurance company has different rules for filing claims.
While some are more lenient than others, it’s important to have access to your office at all times in case you get a call or email that requires immediate attention.
Learn More About Medical Coding
Medical coding is an important part of how a medical office operates. There are six key factors to consider in this post when it comes to planning for this process, and each of them is incredibly important.
Medical coding can help you save time, reduce errors and provide accurate information for your patients.
It’s also a way that an office can organize their patient information, which means it’s essential if you want accurate records of what happened with your patients.
Want more articles like this? Check out our blog!